Introduction: Covid-19 is a highly contagious, rapidly spreading new viral infection syndrome with significant mortality. As with all new diseases we are still in the learning phase. No treatment can be finalized without proper and complete understanding of all components of the disease processes – Epidemiology, Pathophysiology, clinical features in precise details. As far as this disease is concerned there is a sense of urgency. There is a tendency for trying any drug that sounds useful however flimsy the evidence may be. Naturally many drugs are being cleared by the authorities like FDA on urgent basis. Only experience based on observations and data will tell us which of these are better. Trials with head to head comparisons of drugs will take time. This article is prepared with the information that is available at this moment.
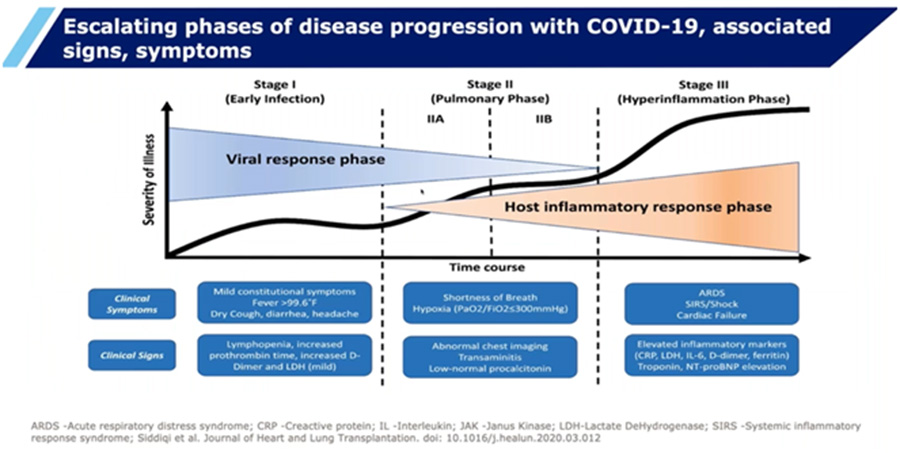
Pathophysiology: Covid-19 is a novel viral infection which came as an unwanted new year gift for 2020. We broadly identify 3 stages of the disease
1. Phase of Infection: Many times asymptomatic; When symptomatic, clinical features resembling common viral infections and flu – Fever, myalgia (body ache) , sore throat, cough, diarrhea, headache lethargy are seen. Loss of smell is an interesting observation. The severity of symptoms is variable and none are specific.
2. Phase of Pulmonary involvement - Complicating Pneumonia – Viral? Bacterial? Interestingly the lung involvement which mimics pneumoniaand is seen after day 10 (in the second week of illness). The person develops cough, has difficulty in breathing (finds it difficult to take a dep breath and hold it in). Interestingly there is a tendency to develop rapid and severe hypoxia (not typical of usual pneumonias). Even those who were relatively comfortable till day 10 seemingly deteriorate quite fast on day 11-14. Initially it was believed to be due to complicating pneumonia. However, we were not sure whether the pneumonia was viral or bacterial but it did not seem to be typical of either. At this point of time giving oxygen through a ventilator seemed to be a good option. Surprisingly the process of ventilation which involves giving oxygen under high tidal volume and high pressure though logical seemingly created more problems and killed many patients. There were 2 possibilities – we were using wrong process or we were using wrong treatment. This is the time I started to interact with my old students and friends (now leaders in their chosen fields) at US, UK and India and periodically got interesting inputs from them. The first change came in the form of modified use of ventilators – 3 modifications were done A) Reduced tidal volume (less traumatic though it gave less Oxygen), B) Paralyzing the patient adequately so that the process of ventilation is unhindered by patient competing with ventilator C) Proning the patient in stages to facilitate better ventilation. All along we firmly believed this was an ongoing form of ARDS. My student in New York (at the peak of mortality) mentioned a chance encounter of the Pulmonologist with a Nephrologist – Nephrologist mentioning increase in cases if AKI he was seeing compared to other viral and bacterial Pneumonias – Why would a pneumonia result in AKI? MOF seemingly followed these problems. Also observed were unexpected Strokes and Myocardial infarctions particularly when they stared to do a Covid test on all admitted patients. About a month ago one of my classmates now in the US contacted me about a family member presenting with a complication of Myopericarditis due to Covid. The very next day NEJM came out with a case report of Myopericarditis with Covid. Clearly we were seeing new and unexpected presentations!
3. Phase of Host Inflammatory response & Cytokine storm: We got the missing link – it had to happen- that the process was not mere infection or inflammation – but involved exaggerated host immune response called “Cytokine storm”. Neutrophil response followed by failed phagocytosis and degranulation and release of ROS caused extensive tissue damage. Complement activation and cell lysis only added to this. Many cytokines including IL-6 are blamed for this phase. The host inflammatory response was so severe that it also triggered kinins and coagulation factors resulting in micro thrombi extensively in microcirculations of various organs – causing depletion of coagulation factors and resultant bleeding (Disseminated Intravascular Coagulation). Such a process in the lung radiologically very closely mimics consolidation (pneumonia) – after all, the process involves a fluid replacing air in the alveoli (inflammatory fluid in pneumonia and blood in hemorrhage). Thrombi caused blocks in microcirculations of many organs – Lung causing “Pneumonia” and “hypoxia” seemingly resistant to oxygenation. It also explained AKI, repeated blockages making dialysis difficult, heart attacks and strokes. Aged people and those with co morbidities like diabetes and hypertension seemed to be more vulnerable. Among 100 persons getting Covid infection 86% seemingly did well. 14% had difficulty in breathing and hypoxia requiring management in the ICU– 12 qualified for ventilator use. Now comes the most interesting part – those who were young and had no comorbidities had 28% mortality as compared to 88% mortality in the elderly group (>65 years) with multiple comorbidities. This difference is hard to explain with only process of infection. But bringing in inflammation triggered thrombosis seemingly explained the things much better.
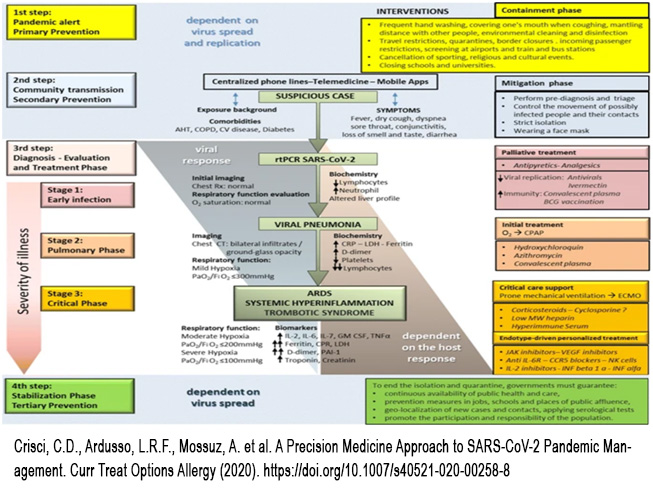
What then is the best course of action? Should we use Antivirals? Antibiotics? Anti-inflammatory drugs? Corticosteroids? Immunomodulators? Well no one drug is confirmed as the best yet! Then we have to look into the prevention – again in the absence of an effective vaccine we can only concentrate on personal hygiene and maybe yet conclusively unproven but seemingly possible effective drugs.
Let us look into the drugs which have been said to be useful in some ways and try to see which slot each of these drugs actually fit in
There is an interesting observation I would like to make: - Anti-inflammatory therapy is much more valuable than antivirals. In fact, patients with rheumatoid arthritis have never been admitted to the Covid departments, because they are on cortisone therapy, which is a great anti-inflammatory. It is also possible that some of these patients are helped by the HCQS they had been taking.
DRUGS & DEVICES TRIED AND THE SLOTS THEY BELONG TO
- Preventing entry of virus:
- HCQS May modify pH of endosomes and prevents viral entry
- Preventing viral growth:
- Remdesivir RNA polymerase inhibitors
- FavipiravirRNA polymerase inhibitors
- Anti-inflammatory
- Corticosteroids
- Interferon IFNα, IFNβ1a
- Monoclonal antibodies
- Tocilizumab/sarilumab - Anti-IL-6
- Siltuximab: Anti-IL-1
- AnakinraAnti-GM-GS
- Gimsilumab Anti-TNFα
- Thalidomide
- Anti-gout Colchicine Tubulin disruption
- Antibiotics: Azithromycin Protease inhibitor
- Thrombosis management: Heparin Anticoagulant
- Organ support:
- Dialysis (AKI)
- Renal protection losartan ARB
- Hypoxia management: High flow oxygen; NIV; Ventilator; Anticoagulant (Thrombosis control)
- Promoting immunity
- Active: Vaccine
- Passive: Convalescent plasma
- ECMO : Support system in the very ill – to help sustain vital functions
The last word is yet to be said!
REFERENCES
- Siddiqui et al Journal of Heart and Lung Transplantation doi: 10_1016/j-healun
- Crisci, C.D., Ardusso, L.R.F., Mossuz, A. et al. A Precision Medicine Approach to SARS-CoV-2 Pandemic Management. Curr Treat Options Allergy (2020). https://doi.org/10.1007/s40521-020-00258-8



